General Discussion
Related: Editorials & Other Articles, Issue Forums, Alliance Forums, Region ForumsAre 'Herd Immunity' Something That The Administration Seems To Be Pushing Now & A Vaccine......
to be available by the end of the year - conflicting goals?
How much of the taxpayers money did Trump give to companies to have a vaccine?
If we achieve 'herd immunity' is a vaccine even necessary?
genxlib
(6,102 posts)If a vaccine is imminent, then every single life lost to a herd immunity strategy would be wasted.
LunaSea
(2,933 posts)for AIDS and herpes, why not give it a shot?
LisaL
(47,367 posts)Even if vaccine becomes available, it's unlikely to be highly efficient. And apparently it's unlikely to be fully tested as well.
TexasProgresive
(12,703 posts)Immunity in the herd usually by vaccination.
This is just more idiots throwing spaghetti at the wall.
Celerity
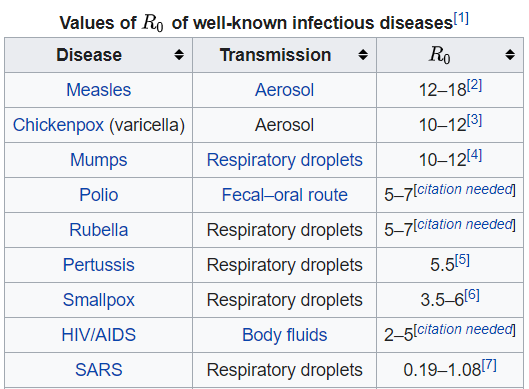
(54,005 posts)herd immunity levels for one disease do not mean the same levels are required for another.
R0, or the basic reproduction number/rate, refers to the contagiousness and transmissibility of infectious pathogens. R0 varies depending on a variety of factors and is critical in public health management to ensure infectious epidemics (or global pandemics) are controlled.
If the R-naught is 1.5.you need a 33.3% exposure rate to hit herd immunity
If the R-naught is 2.0 you need a 50% exposure rate to hit herd immunity.
If it is 2.5, then 60% is need to reach herd immunity
If it is 3.0, 66.7% exposure rate needed
If the R-naught drops under 1.0 and sustains at that level, the viral disease will burn out
The rates generally being tossed out for months for COVID-19 are 1.5 to 3.0 (some very early, now debunked, alarmists were saying it could be as high as 5 or 6.0 or even 7.0), with a consensus average around 2.0 to 2.5
R-naught also is not stable, it is fluid and can go up and down as things shake out.
The only way to truly know when herd immunity is reached is via massive antibody and t-cell testing and/or when the disease basically falls off and stops or nearly stops.
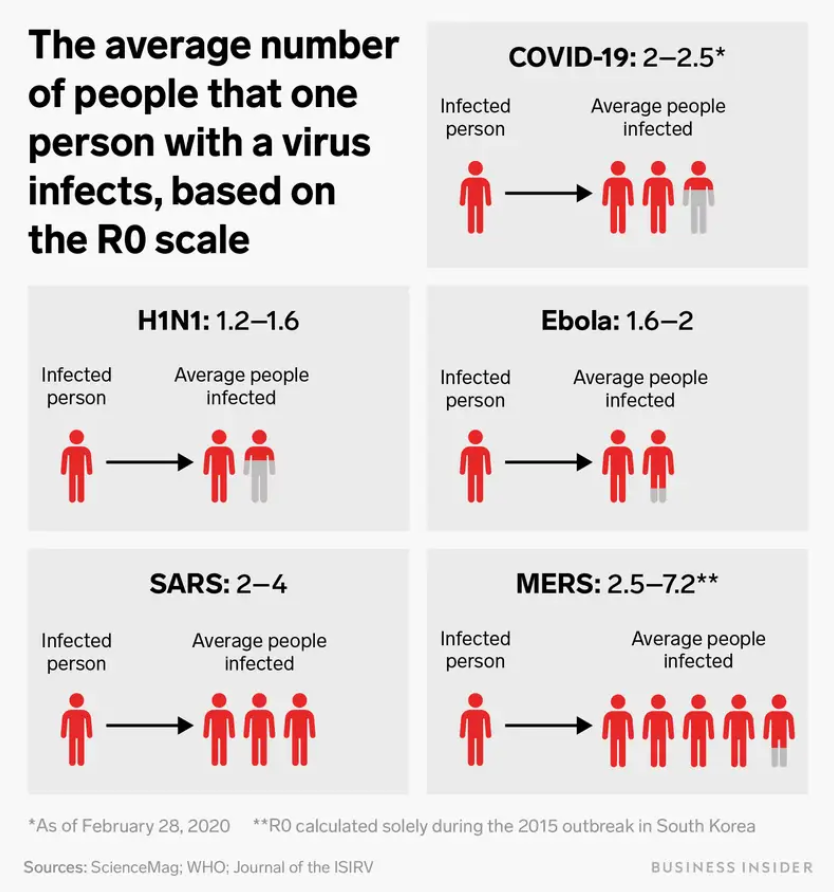
An average coronavirus patient infects at least 2 others. To end the pandemic, that crucial metric needs to drop below 1 — here's how we get there.
A crucial metric called R0, pronounced R-naught, represents how many people an average person with a virus infects.
The coronavirus has an R0 of roughly 2 to 2.5, meaning that each new person spreads the disease to about 2.2 people on average.
That makes COVID-19 more contagious than the seasonal flu.
But a disease's R0 isn't fixed — it can decrease with the right preventive measures. Bringing it below 1 would end the pandemic.
https://www.businessinsider.com/coronavirus-contagious-r-naught-average-patient-spread-2020-3?r=US&IR=T
A crucial step in reigning in the coronavirus pandemic is determining exactly how contagious it is. That comes down to one crucial metric: the R0 (pronounced R-naught).
R0 refers to the average number of people that one sick person goes on to infect in a group that has no immunity. Experts use it to predict how far and how fast a disease will spread, and the number can also inform policy decisions about how to contain an outbreak.
"R0 is a population-based determination that helps you to decide, is the outbreak taking off, leveling off, or diminishing?" Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, said in a February interview hosted by the Journal of the American Medical Association.
The R0 of the coronavirus so far seems to hover around 2 to 2.5, according to the World Health Organization. A study of the poorly contained outbreak on the Diamond Princess cruise ship revealed an R0 consistent with those estimates: 2.2.
That means it's more contagious than the seasonal flu, but less contagious than measles.
"It is a virus that is quite good at transmitting from one person to another," Fauci said.
How R0 works
A given pathogen's R0 value changes with place and time.
"There is no R0 — there is an R0 in a population," Elizabeth Halloran, a biostatistician at Fred Hutchinson Cancer Research Center and University of Washington, told Business Insider. A recent CDC study found that the coronavirus's R0 was as high as 5.7 in the early days of its Wuhan outbreak.
An R0 value of 1 means the average person who gets that disease will transmit it to one other person; in that case, the disease is spreading at a stable rate. An R0 of more than 1 means the disease spreads exponentially.
When experts strategize about how to end the pandemic, their goal is to bring the R0 below 1, which would put the coronavirus in decline until it dies out.
snip
What Is R0?: Gauging Contagious Infections
https://www.healthline.com/health/r-nought-reproduction-number
snip
How is the R0 of a disease calculated?
The following factors are taken into account to calculate the R0 of a disease:
Infectious period
Some diseases are contagious for longer periods than others. For example, according to the Centers for Disease Control and Prevention, adults with the flu are typically contagious for up to eight days, while children can be contagious for up to two weeks. The longer the infectious period of a disease, the more likely an infected person is to spread the disease to other people. A long period of infectiousness will contribute to a higher R0 value.
Contact rate
If a person who’s infected with a contagious disease comes into contact with many people who aren’t infected or vaccinated, the disease will spread more quickly. If that person remains at home, in a hospital, or otherwise quarantined while they’re contagious, the disease will spread more slowly. A high contact rate will contribute to a higher R0 value.
Mode of transmission
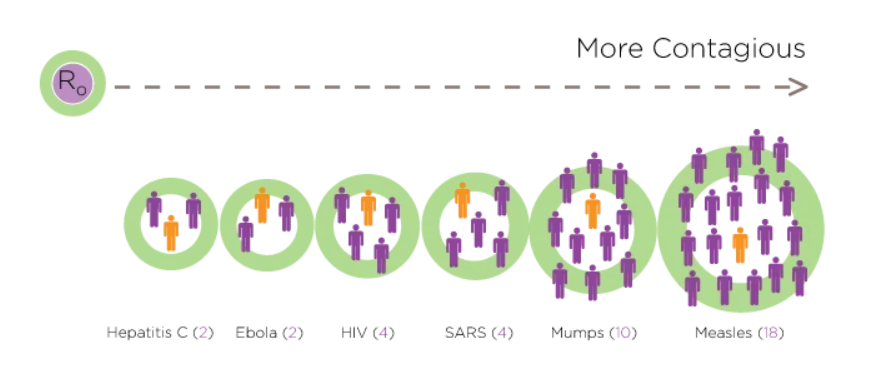
The diseases that spread most quickly and easily are the ones that can travel through the air, such as the flu or measles. Physical contact with an infected person isn’t necessary for the transmission of such conditions. You can catch the flu from breathing near someone who has the flu, even if you never touch them.
In contrast, diseases that are transmitted through bodily fluids, such as Ebola or HIV, aren’t as easy to catch or spread. This is because you need to come into contact with infected blood, saliva, or other bodily fluids to contract them. Airborne illnesses tend to have a higher R0 value than those spread through contact.
What conditions are measured by R0?
R0 can be used to measure any contagious disease that may spread in a susceptible population. Some of the most highly contagious conditions are measles and the common flu. More serious conditions, such as Ebola and HIV, spread less easily between people.
This illustration shows some commonly known diseases and their estimated R0 values.
snip
Volume 25, Number 1—January 2019
Perspective
Complexity of the Basic Reproduction Number (R0)
https://wwwnc.cdc.gov/eid/article/25/1/17-1901_article
Abstract
The basic reproduction number (R0), pronounced “R naught,” is intended to be an indicator of the contagiousness or transmissibility of infectious and parasitic agents. R0 is often encountered in the epidemiology and public health literature and can also be found in the popular press (1–6). R0 has been described as being one of the fundamental and most often used metrics for the study of infectious disease dynamics (7–12). An R0 for an infectious disease event is generally reported as a single numeric value or low–high range, and the interpretation is typically presented as straightforward; an outbreak is expected to continue if R0 has a value >1 and to end if R0 is <1 (13). The potential size of an outbreak or epidemic often is based on the magnitude of the R0 value for that event (10), and R0 can be used to estimate the proportion of the population that must be vaccinated to eliminate an infection from that population (14,15). R0 values have been published for measles, polio, influenza, Ebola virus disease, HIV disease, a diversity of vectorborne infectious diseases, and many other communicable diseases (14,16–18).
The concept of R0 was first introduced in the field of demography (9), where this metric was used to count offspring. When R0 was adopted for use by epidemiologists, the objects being counted were infective cases (19). Numerous definitions for R0 have been proposed. Although the basic conceptual framework is similar for each, the operational definitions are not always identical. Dietz states that R0 is “the number of secondary cases one case would produce in a completely susceptible population” (19). Fine supplements this definition with the description “average number of secondary cases” (17). Diekmann and colleagues use the description “expected number of secondary cases” and provide additional specificity to the terminology regarding a single case (13).
In the hands of experts, R0 can be a valuable concept. However, the process of defining, calculating, interpreting, and applying R0 is far from straightforward. The simplicity of an R0 value and its corresponding interpretation in relation to infectious disease dynamics masks the complicated nature of this metric. Although R0 is a biological reality, this value is usually estimated with complex mathematical models developed using various sets of assumptions. The interpretation of R0 estimates derived from different models requires an understanding of the models’ structures, inputs, and interactions. Because many researchers using R0 have not been trained in sophisticated mathematical techniques, R0 is easily subject to misrepresentation, misinterpretation, and misapplication. Notable examples include incorrectly defining R0 (1) and misinterpreting the effects of vaccination on R0 (3). Further, many past lessons regarding this metric appear to have been lost or overlooked over time. Therefore, a review of the concept of R0 is needed, given the increased attention this metric receives in the academic literature (20). In this article, we address misconceptions about R0 that have proliferated as this metric has become more frequently used outside of the realm of mathematical biology and theoretic epidemiology, and we recommend that R0 be applied and discussed with caution.
Variations in R0
snip
Features, Evaluation and Treatment Coronavirus (COVID-19)
https://www.ncbi.nlm.nih.gov/books/NBK554776/
snip
Transmission
Because the first cases of the CoVID-19 disease were linked to direct exposure to the Huanan Seafood Wholesale Market of Wuhan, the animal-to-human transmission was presumed as the main mechanism. Nevertheless, subsequent cases were not associated with this exposure mechanism. Therefore, it was concluded that the virus could also be transmitted from human-to-human, and symptomatic people are the most frequent source of COVID-19 spread. The possibility of transmission before symptoms develop seems to be infrequent, although it cannot be excluded. Moreover, there are suggestions that individuals who remain asymptomatic could transmit the virus. This data suggests that the use of isolation is the best way to contain this epidemic.
As with other respiratory pathogens, including flu and rhinovirus, the transmission is believed to occur through respiratory droplets from coughing and sneezing. Aerosol transmission is also possible in case of protracted exposure to elevated aerosol concentrations in closed spaces. Analysis of data related to the spread of SARS-CoV-2 in China seems to indicate that close contact between individuals is necessary. The spread, in fact, is primarily limited to family members, healthcare professionals, and other close contacts.
Based on data from the first cases in Wuhan and investigations conducted by the China CDC and local CDCs, the incubation time could be generally within 3 to 7 days and up to 2 weeks as the longest time from infection to symptoms was 12.5 days (95% CI, 9.2 to 18). This data also showed that this novel epidemic doubled about every seven days, whereas the basic reproduction number (R0 - R naught) is 2.2. In other words, on average, each patient transmits the infection to an additional 2.2 individuals. Of note, estimations of the R0 of the SARS-CoV epidemic in 2002-2003 were approximately 3.
snip
“When will it be over?”: An introduction to viral reproduction numbers, R0 and Re
https://www.cebm.net/covid-19/when-will-it-be-over-an-introduction-to-viral-reproduction-numbers-r0-and-re/
The basic reproduction number
The basic reproduction number is defined as the number of cases that are expected to occur on average in a homogeneous population as a result of infection by a single individual, when the population is susceptible at the start of an epidemic, before widespread immunity starts to develop and before any attempt has been made at immunization. So if one person develops the infection and passes it on to two others, the R0 is 2.
If the average R0 in the population is greater than 1, the infection will spread exponentially. If R0 is less than 1, the infection will spread only slowly, and it will eventually die out. The higher the value of R0, the faster an epidemic will progress.
R0 is estimated from data collected in the field and entered into mathematical models. The estimated value depends on the model used and the data that inform it.
R0 is affected by:
the size of the population and the proportion of susceptible people at the start;
the infectiousness of the organism;
the rate of disappearance of cases by recovery or death, the first of which depends on the time for which an individual is infective;
The larger the population, the more people are susceptible, and the more infective the virus, the larger R0 will be for a given virus; the faster the rate of removal of infected individuals, by recovery or death, the smaller R0 will be.
The zero in “R zero” means that it is estimated when there is zero immunity in the population, even though not everyone will necessarily be susceptible to infection, although that is the usual assumption. In an epidemic with a completely new virus, the earlier the measurements are made the nearer the calculated value is likely to be to the true value of R0, assuming high-quality data. For this reason, it is better to talk about the transmissibility of the virus at the time that it is measured, using a different symbol, Re, the effective reproduction number.
The effective reproduction number, Re
The effective reproduction number, Re, sometimes also called Rt, is the number of people in a population who can be infected by an individual at any specific time. It changes as the population becomes increasingly immunized, either by individual immunity following infection or by vaccination, and also as people die.
Re is affected by the number of people with the infection and the number of susceptibles with whom infected people are in contact. People’s behaviour (e.g. social distancing) can also affect Re.
The number of susceptibles falls as people die or become immunized by exposure. The sooner people recover or die, the smaller the value of Re will be at any given time.
Unfortunately, the symbol R0 is often used in publications when Re is meant. This can be confusing.
Herd immunity
Initial reports suggested that one of the UK Government’s strategies in tackling the pandemic was to allow the virus to spread within the community, in a controlled way, so that immunity, so-called herd immunity, could develop across the population. However, the health secretary, Matt Hancock, later said that this was not part of the UK response to the virus. In contrast, other countries, such as Sweden, have responded to the pandemic in ways that avoid full lockdown. The problem with leaving people to catch the infection spontaneously, leading to herd immunity, is that the death rate would increase as a result. For example, on 10 April, the number of confirmed cases in Sweden was 9685 with 870 deaths (9.0%), compared with Norway with 6219 confirmed cases and 108 deaths (1.7%) and Denmark with 5830 confirmed cases and 237 deaths (4.4%).
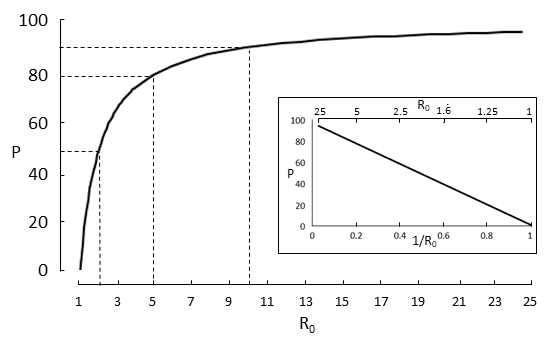
R0 predicts the extent of immunization that a population requires if herd immunity is to be achieved, the spread of the infection limited, and the population protected against future infection. To prevent sustained spread of the infection the proportion of the population that has to be immunized (Pi) has to be greater than 1 − 1/R0. The relation between Pi and 1 – 1/R0 is shown in Figure 1.
For example, if R0 = 2, immunization needs to be achieved in 50% of the population. However, if R0 = 5 the proportion rises steeply, to 80%. Beyond that the rise is less steep; an increase in R0 to 10 increases the need for immunization to 90%. Measles has an R0 greater than 10, which is why immunization of a large proportion of the population is so important in preventing the disease.
Thus, if R0 is 10, a child with measles will infect 10 others if they are susceptible. When other children become immune the infected child who encounters 10 children will not be able to infect them all; the number infected will depend on Re. When immunity is 90% or more the chances that the child will meet enough unimmunized children to pass on the disease falls to near zero, and the population is protected.
Hugin
(37,622 posts)and looking back once the pandemic has gone completely and irrevocably out of control and saying, "Eh, we tried. There was nothing to be done."
Sort of like mass shootings in Elementary Schools and oiling up the Gulf of Mexico with spills.
I prefer to call it the 'Wall Street' plan and it's what they've been doing all along. This is nothing new.
hlthe2b
(113,211 posts)be possible. The Oxford vaccine does have the advantage of stimulating both antibody AND t-cell response so it may well have longer protection, but thus far we have no reason to conclude that long term immunity is even possible--in fact to the contrary based on neutralizing antibody alone.
Only one infectious disease has ever been eradicated--smallpox and it would never have been so had there not been essentially lifelong immunity conferred from both natural infection AND approaching such from the vaccine.
That is why, we've not yet been able to eradicate measles. We have a good vaccine, but immunity is not lifelong and the virus is so infectious herd immunity would have to be almost impossibly high to totally eradicate it. We can eliminate risk by lowering transmission to a certain level as has been achieved from time to time in the western hemisphere, but elimination is not eradication.
magicarpet
(18,464 posts)He wants all schools and colleges open,
He wants retail open,
He wants restaurants and liquor bars open,
He wants churches fully open,
And he wants the cash registers ringing loud and clear so the economy fully recovers before election day.
The economy must fully recover,.. that is his line in the sand,.. then trDump thinks he will win his second term by a landslide.
regnaD kciN
(27,543 posts)It requires around 70% of the population to contract the virus. If we use the most-optimistic numbers (from the COVID Machine Learning Project) as to how many may have contracted it, including those who were asymptomatic, it works out that achieving herd immunity will result in around 900,000 American deaths. And that’s an optimistic scenario, because:
1) It assumes that those 900K “considerately” die at a gradual enough rate that we don’t see hospitals being overrun as they were in March and April, which would result in lots of people who could have survived the illness dying from being unable to receive care.
2) It accepts the Project’s assumption of about 80% asymptomatic cases, when no one really knows for sure. If they’re off by even a small percentage, the death toll would top one million. If only half of cases are asymptomatic, we’re looking at over two million. And most experts believe that less than half are asymptomatic.
3) It also assumes long-term immunity, which may be a faulty assumption considering evidence of reinfection of people who already had the disease, about three months later. Granted, so far, it seems any such cases have been asymptomatic, but what if many/most aren’t? There’s a reason we’ve never developed herd immunity to the common cold.
